Authors: Annie Arens MD, Jon Cole MD, and Justin Corcoran MD
Internal Reviewer: Samuel Stellpflug MD
External Reviewer: Daniel Sessions, MD
Intro
In the last few months, Covid-19 has developed into a worldwide pandemic.1 Unfortunately, this has led to multiple attempts to use home remedies as a treatment or preventative measure. These have led to deaths independent of the virus, notably the deaths of over 100 people in Iran from methanol poisoning.2 In the midst of all of this, there have been widespread media reports of the possibility of using chloroquine or hydroxychloroquine to treat patients with Covid-19. This arose after trials in China, using small numbers of patients, appeared to show benefit from chloroquine.3 A small French study subsequently showed IMPROVED VIRAL CLEARANCE after 6 days of treatment hydroxychloroquine, and even better with a combination of hydroxychloroquine and azithromycin (we are still waiting on any clinical data).4 Following this, the US president Donald Trump stated during a discussion about hydroxychloroquine that, “I feel good about it. That’s all it is, just a feeling, you know, smart guy. I feel good about it.”5 He also tweeted a positive statement about it:
It should not come as a surprise, then, that death from chloroquine overdose has now joined the ranks of accidental poisonings secondary to this pandemic. An elderly couple, having heard that chloroquine is helpful for treating Covid-19, ingested chloroquine phosphate that was intended for aquarium use; unfortunately, the man died and his wife is in critical care.6
Discussion
How do chloroquine/hydroxychloroquine work?
- To treat malaria?
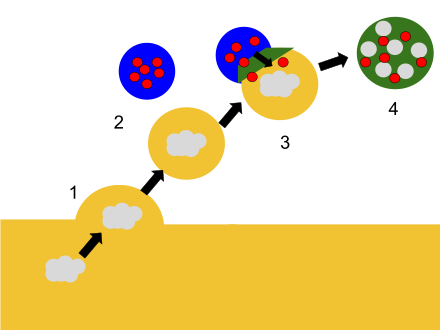
The therapeutic mechanism of the drug, as an antimalarial, is that it interferes with digestive (food) vacuole function within sensitive malaria parasites by increasing the pH and interfering with lysosomal degradation of hemoglobin.7 Malaria parasites consume hemoglobin, which produces free heme, and free heme is toxic. Malaria use their lysosomes to detoxify heme to the inert hemozoin. Hydroxychloroquine (and all of the amino alcohols and 4-aminoquinoline drugs like chloroquine) inhibit the ability of the malaria parasite to detoxify heme, heme accumulates, and the parasite dies.7,8
If you’re like us and you haven’t thought about food vacuoles and lysosomes in a while – here’s a diagram. The gray cloud is food, the yellow circle is the food vacuole performing endocytosis, the blue circles with red dots are the lysosomes, and the green blob is their combined digestive state. Chloroquine and quinidine concentrate in the yellow food vacuoles to treat Malaria.
- To treat rheumatologic diseases?
For rheumatologic conditions, hydroxychloroquine works by yet another mechanism – in this case it is grouped with other disease-modifying antirheumatic drugs (DMARDs). DMARDs are a large group of drugs that can be divided into 2 subgroups; conventional synthetic (csDMARDs) and biologic (bDMARD). bDMARDs are the expensive new drugs that end in “-cept” or “-mab” and are advertised on TV. csDMARDs can be further divided up; in hydroxychloroquine’s case, it works by blocking toll-like receptors (TLR) on plasmacytoid dendritic cells (PDCs).9 TLRs recognize DNA-containing immune complexes – sounds like a rheumatologic disease, right? – and when activated lead to the production of interferon, causing dendritic cells to mature and present antigens to T cells. By blocking TLRs, hydroxychloroquine slows the inflammatory and autoimmune responses to treat diseases like Lupus.9 - To treat the dread pirate coronavirus?
One proposed mechanism for treating viruses, and specifically coronaviruses, is largely the same as for treating malaria – alkalinization of lysosomes, thus impairing entry into the cell.10 Another mechanism is that these drugs may also interfere with glycosylation of cell surface receptors, again interfering with viral entry into the cell.11 Specifically, in the case of SARS-CoV (the virus behind the SARS outbreak), it was proposed that the glycosylation of ACE2, the cell surface target of SARS-CoV, was inhibited by chloroquine.12 This (ACE2) is also the purported receptor for SARS-CoV-2 (the virus behind the COVID-19 pandemic).13 Interest in chloroquine and hydroxychloroquine as a possible therapeutic agent for SARS-CoV-2 is also supported by in vitro evidence of efficacy against SARS-CoV.12,14 This has been further supported by low-quality evidence of benefit in humans; these studies are confounded by low numbers of patients, and in one case, significant (and potentially biased) drop-out in the treatment group.3,4
- To kill you in overdose?
- Both drugs are structurally similar to quinine and as such have similar mechanisms of action and toxicity.15 Specifically:
- Inhibition of sodium channels16
- Inhibition of potassium (hERG) channels15,16
- Profound hypokalemia from intracellular shifting, also contributing to dysrhythmias.15–17
- Hydroxychloroquine also results in inhibition of ATP-sensitive K+ channels on pancreatic beta-islet cells causing hypoglycemia.18
- So basically… it’s like overdosing on a class I antidysrhythmic (e.g. quinidine) and a sulfonylurea at the same time.
- Both drugs are structurally similar to quinine and as such have similar mechanisms of action and toxicity.15 Specifically:
You have a patient who overdosed on hydroxychloroquine to REALLY cure their coronavirus…now what?
If there’s one important thing (and there are many) to remember about these overdoses, it is that they can go badly – FAST. Cardiovascular effects in significant overdose are relatively rapid, typically occurring within several minutes – up to 3 hours.15,19,20 This rapidity makes sense knowing peak serum concentrations are reached within 1.5-3 hours.20 If you think about how these medications cause cardiotoxicity, the clinical effects are fairly predictable:20
- Negative inotropy
- Inhibition of diastolic depolarization
- Slowed cardiac conduction
- Prolonged refractory period
- Raised electrical threshold
Put them all together, and what have you got? Decreased cardiac contractility, impaired cardiac conduction, decreased excitability, and reentrant tachycardias.20
Patients may exhibit profound hypotension and cardiovascular collapse, with both reduced cardiac output and vasodilation to blame in some patients.16,20 This is a great time to use your shiny point of care ultrasound skills to help decipher what is contributing to your patient’s shock state. In fact, just do this will all of your sick overdose patients. Even better, all of your sick patients.
Not surprisingly, ventricular dysrhythmias are king with these overdoses. As you may expect, patients may have QRS and QT prolongation with the expected decompensation to ventricular dysrhythmias and potentially torsade des pointes.16,20,21 Patients may have a predisposition to ventricular tachycardia and fibrillation because of the prolonged refractory period.22
What other badness can you see? Seizures – don’t forget that you’ve also got sodium channels in the central nervous system that can be affected in overdose too, and cause seizures.23 Also, patients may have significant CNS depression with associated respiratory depression or apnea.23 Let’s not forget about hypoglycemia and profound hypokalemia; we’re talking 5.3 mEq/L to 2.1 mEq/L over the course of an hour in one patient.16 As a matter of fact, the degree of hypokalemia is predictive of the severity of toxicity.20
Another bummer in chronic use of these medications is irreversible hearing and vision loss. Though the exact mechanism is still unclear, chronic use is associated with initial parafoveal photoreceptor loss with eventual diffuse receptor loss across the entire macula.24
Can you predict who is going to die?
If you were in France in the 1980’s the greatest predictors of fatality from chloroquine overdose include:21
- Ingestion > 5g;
- Initial systolic BP < 80
- QRS duration > 0.12s
- Other predictive factors include: ventricular dysrhythmias and a blood concentration > 8 mg/ml22
Treatment in ACUTE overdose
Again, a lot of this will be intuitive based upon the mechanism of toxicity for these medications, but there are a couple of special considerations for these overdoses. We will not discuss some of the more chronic changes including: hearing and vision loss, as well as hypersensitivity reactions including cardiomyopathy.
- Supportive care. And call Poison Control! Duh. This will get you 99% of the way in almost any overdose, even if there is an antidote available. For these overdoses, however, you should think about being aggressive early, including obtaining multiple points of IV access, early EKG and labs (especially a point of care blood glucose), bedside ultrasound, and potential early intubation for patients with CNS depression.22
- GI decontamination. This is always a controversial topic. These drugs undergo very rapid absorption, with astronomical volumes of distribution (800 L/kg for hydroxychloroquine).16 Outside of an initial dose of activated charcoal, in the appropriate patient, there is unlikely to be a whole lot of benefit to something like whole bowel irrigation. Chloroquine does bind charcoal, although the rapid absorption may prevent administering it early enough to make a difference.25 This may be one of those rare patients you actually dig out the Ewald tube.
- QRS prolongation and ventricular dysrhythmias. Please don’t forget your usual ACLS algorithms for patients in cardiac arrest. Chest compressions >>> academic discussions about high dose diazepam.
- Sodium bicarbonate. This is our usual go-to to treat QRS prolongation and ventricular dysrhythmias secondary to sodium channel blockade. While the exact mechanism of how it actually works is unclear, and differs by the specific toxin, it is likely the result of simply increased sodium concentration, increased pH, or a combination thereof.26 For chloroquine or hydroxychloroquine, sodium bicarbonate is a reasonable first choice to treat QRS prolongation (we usually recommend 1-3 amps of sodium bicarbonate IV to start, with immediate repeat EKG’s to evaluate for QRS narrowing and repeat doses as needed, rather than infusions). This has to be weighed, however, by the degree of hypokalemia. Don’t forget that this may further shift potassium into cells. If you’re looking for an alternative to sodium bicarbonate to treat ventricular dysrhythmias, consider lidocaine as an alternative. Also, hypertonic saline is a potential alternative (that would avoid intracellular potassium shift), although we were unable to identify any literature reports of its use for this purpose.27
- Lidocaine. Lidocaine has been used to treat patients successfully with ventricular arrhythmias following hydroxychloroquine overdose.16,28 Does it make sense to treat what amounts to a 1a overdose with a 1b antidysrhythmic? Sure. While lidocaine blocks sodium channels in the open and inactive states (which sounds bad), it dissociates from the sodium channel during diastole thus allowing for rapid recovery.29 This is especially true at faster heart rates, thus making it a good choice of antidysrhythmic.
- QT(c) prolongation. These overdoses are tricky, because you’ve got multiple contributing mechanisms, including potassium channel blockade AND hypokalemia. And yes, patients have developed torsades des pointes with chloroquine in particular.21 The treatment of QT prolongation in these overdoses does not differ from your usual treatment.
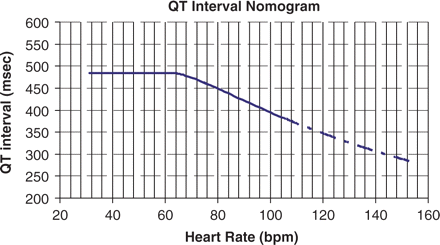
- QT nomogram. Hand calculating a QT interval and plotting it against the patient’s HR – this will give you a more accurate assessment of a patient’s risk of dysrhythmia.30,31
- Electrolyte replacement. Particularly potassium. Potassium levels have been shown to fall dramatically and rapidly16,17, and while it is the result of intracellular shift, rather than total body depletion, cardiac myocytes still abhor sudden changes in potassium concentrations. How quickly it is safe to replace potassium is up for debate. Regardless, check electrolytes (don’t forget magnesium, phos, and calcium) often, and replace liberally. Rebound hyperkalemia is a concern16, but it is a lot easier to treat hyperkalemia in an alive patient.
- Magnesium? Maybe? It is unclear if magnesium infusions are really necessary for JUST QTc prolongation.
- QT nomogram. Hand calculating a QT interval and plotting it against the patient’s HR – this will give you a more accurate assessment of a patient’s risk of dysrhythmia.30,31
- Torsades des Pointes.
- Defibrillate unstable patients!
- Magnesium. Magnesium sulfate IV infusion (2g) is a well established treatment to ABORT Torsades des Pointes. With the proposed mechanism of decreasing calcium influx and thus lowering the amplitude of early afterdepolarizations and terminating arrhythmias.
- Overdrive pacing. You must have a patient who is currently OUT of TdP, and this is hard to pull off without an intravenous pacer, but is possible with transcutaneous pacing. The idea here is to override an ectopic pacemaker changing the pattern of repolarization and thus disrupting a re-entrant tachycardia. Essentially, a pacer is used to increase the patient’s heart rate to 10-20 bpm greater than the patient’s native rate.
- Pressor choice. Epinephrine to start. Where does this recommendation come from? No one will be surprised to know there is little controlled research into the treatment of these overdoses. But there is one, well sort of. Riou et al prospectively investigated 11 patients with > 5g of chloroquine ingestion. Each patient received 1) early intubation and NGT placement for gastric aspiration; 2) epinephrine 0.25 mcg/kg/min, increasing by 0.25 mcg/kg/min until an adequate systolic BP (> 100 mmHg) was reached; 3) diazepam 2 mg/kg IV. Ten of these eleven patients survived, as compared to one of the historical controls.21 Mechanistically, epinephrine is a great choice given it’s inotropic effects as well as potent vasoconstriction. But norepinephrine is likely an equally good choice to start with for the same reasons. It is the Frank’s Red Hot of pressors – just put that sh*t on everything.
- Diazepam. A METRIC SH*T – TON OF DIAZEPAM. High-dose diazepam (especially in conjunction with epinephrine) is recommended to augment the treatment of hypotension and dysrhythmias. This is best studied in chloroquine toxicity.21,32 There are several proposed mechanisms of action: 1) central antagonism; 2) anticonvulsant effect; 3) antidysrhythmic effect by electrophysiologic action inverse to chloroquine; 4) pharmacokinetic interaction between diazepam and chloroquine; and 5) decreased chloroquine-induced vasodilation.15 Don’t forget that there are specific cardiac diazepam receptors (why? No idea).
- The recommended dose comes right out of Goldfranks:15 2 mg/kg IV over 30 minutes followed by 1-2 mg/kg/day for 2-4 days.
- Where this falls apart: Diazepam doesn’t play well with other medications and may cause precipitation and is notorious for sticking to IV tubing, so it is the opinion of the authors that this can probably be divided into hourly push doses.
- Is there anything special about diazepam over other benzodiazepines? Maybe? As above, there are some mechanisms special to diazepam that may favor its use. There aren’t any specific studies looking into this, but it certainly seems reasonable to substitute and augment diazepam with other benzodiazepines and sedatives like propofol. Interestingly, one group actually gave these huge doses of diazepam to 23 patients who were not intubated.32 Baller.
- Glucose: Remember that these patients can get hypoglycemic. This may be due to increased insulin release from pancreatic beta cells secondary to a sulfonylurea-like inhibition of ATP-sensitive potassium channels, although evidence is conflicting.18,33,34 In any case, treatment with dextrose is indicated if hypoglycemic, and octreotide may be considered by analogy with sulfonylurea overdose (but has no literature evidence supporting it for chloroquine/hydroxychloroquine specifically).35
- Intravenous Lipid Emulsion (ILE). No matter how you slice it, ILE is controversial for most things, with the exception of local anesthetic toxicity. In patients with refractory hypotension, there are reports of patients improving with intravenous lipid emulsion.36,37 So, as usual, something to consider when you have a very sick patient who is refractory to maximal supportive care.
- VA ECMO. On a brief literature search, we identified only a single case of chloroquine poisoning treated with VA-ECMO; this patient survived her poisoning.38 It is reasonable to expect that a patient with refractory dysrhythmias or severely depressed cardiac function might benefit from VA ECMO. We would argue however, that this is UNLIKELY to benefit patients with refractory VASOPLEGIC shock, because, well…ECMO doesn’t work that way.
Don’t forget:
- Wash your hands
- Stop smoking
- Wear your seatbelt
- Wear a helmet when you’re riding a bike
- Dr. Daniel Sessions did the math: it would take > 11L of commercially available tonic water to get a therapeutic dose of quinine…which is not the same as chloroquine…which is not the same as hydroxychloroquine. So while a G&T is a great drink – it won’t help your coronavirus. That said, stay thirsty, my friends.
References:
1. Chappell B. Coronavirus: COVID-19 Is Now Officially A Pandemic, WHO Says [Internet]. NPR.org. 2020 [cited 2020 Mar 24];Available from: https://www.npr.org/sections/goatsandsoda/2020/03/11/814474930/coronavirus-covid-19-is-now-officially-a-pandemic-who-says
2. Iran: Death toll from toxic alcohol rises to 180 [Internet]. [cited 2020 Mar 24];Available from: https://www.aa.com.tr/en/health/iran-death-toll-from-toxic-alcohol-rises-to-180/1771659
3. Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends 2020;14(1):72–3.
4. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020;105949.
5. Facher L, Florko N, Garde D. Trump says his belief in one potential coronavirus drug is “just a feeling” [Internet]. STAT. 2020 [cited 2020 Mar 24];Available from: https://www.statnews.com/2020/03/20/trump-coronavirus-drug-just-a-feeling/
6. A man died after ingesting a substance he thought would protect him from coronavirus [Internet]. NBC News. 2020 [cited 2020 Mar 24];Available from: https://www.nbcnews.com/health/health-news/man-dies-after-ingesting-chloroquine-attempt-prevent-coronavirus-n1167166
7. Pussard E, Verdier F. Antimalarial 4-aminoquinolines: mode of action and pharmacokinetics. Fundam Clin Pharmacol 1994;8(1):1–17.
8. Warhurst DC. Antimalarial drugs. An update. Drugs 1987;33(1):50–65.
9. Sacre K, Criswell LA, McCune JM. Hydroxychloroquine is associated with impaired interferon-alpha and tumor necrosis factor-alpha production by plasmacytoid dendritic cells in systemic lupus erythematosus. Arthritis Res Ther 2012;14(3):R155.
10. Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents 2020;105932.
11. Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 2020;30(3):269.
12. Vincent MJ, Bergeron E, Benjannet S, et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J 2005;2(1):1–10.
13. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell [Internet] 2020;Available from: http://dx.doi.org/10.1016/j.cell.2020.02.052
14. In vitro inhibition of severe acute respiratory syndrome coronavirus by chloroquine. Biochem Biophys Res Commun 2004;323(1):264–8.
15. Barry JD. Antimalarials. In: Nelson L, Howland MA, Lewin N, Smith S, Goldfrank L, Hoffman R, editor. Goldfrank’s Toxicologic Emergencies,. p. 836–49.
16. de Olano J, Howland MA, Su MK, Hoffman RS, Biary R. Toxicokinetics of hydroxychloroquine following a massive overdose. Am J Emerg Med 2019;37(12):2264.e5–2264.e8.
17. Jordan P, Brookes JG, Nikolic G, Le Couteur DG. Hydroxychloroquine overdose: toxicokinetics and management. J Toxicol Clin Toxicol 1999;37(7):861–4.
18. Davis TM. Antimalarial drugs and glucose metabolism. Br J Clin Pharmacol 1997;44(1):1–7.
19. Isbister GK, Dawson A, Whyte IM. Hydroxychloroquine overdose: a prospective case series. Am. J. Emerg. Med. 2002;20(4):377–8.
20. Marquardt K, Albertson TE. Treatment of hydroxychloroquine overdose. Am J Emerg Med 2001;19(5):420–4.
21. Riou B, Barriot P, Rimailho A, Baud FJ. Treatment of severe chloroquine poisoning. N Engl J Med 1988;318(1):1–6.
22. Ling Ngan Wong A, Tsz Fung Cheung I, Graham CA. Hydroxychloroquine overdose: case report and recommendations for management. Eur J Emerg Med 2008;15(1):16–8.
23. Jaeger A, Sauder P, Kopferschmitt J, Flesch F. Clinical features and management of poisoning due to antimalarial drugs. Med Toxicol Adverse Drug Exp 1987;2(4):242–73.
24. de Sisternes L, Hu J, Rubin DL, Marmor MF. Localization of damage in progressive hydroxychloroquine retinopathy on and off the drug: inner versus outer retina, parafovea versus peripheral fovea. Invest Ophthalmol Vis Sci 2015;56(5):3415–26.
25. Kivistö KT, Neuvonen PJ. Activated charcoal for chloroquine poisoning. BMJ. 1993;307(6911):1068.
26. Bruccoleri RE, Burns MM. A Literature Review of the Use of Sodium Bicarbonate for the Treatment of QRS Widening. J Med Toxicol 2016;12(1):121–9.
27. Kolecki PF, Curry SC. Poisoning by sodium channel blocking agents. Crit Care Clin 1997;13(4):829–48.
28. Chen C-Y, Wang F-L, Lin C-C. Chronic hydroxychloroquine use associated with QT prolongation and refractory ventricular arrhythmia. Clin Toxicol 2006;44(2):173–5.
29. Sztajnkrycer. Local anesthetics. In: Nelson L, Howland MA, Lewin N, Smith S, Goldfrank L, Hoffman R, editor. Goldfrank’s Toxicologic Emergencies, 11th ed. p. 994–1003.
30. Isbister GK, Page CB. Drug induced QT prolongation: the measurement and assessment of the QT interval in clinical practice. Br J Clin Pharmacol 2013;76(1):48–57.
31. Chan A, Isbister GK, Kirkpatrick CMJ, Dufful SB. Drug-induced QT prolongation and torsades de pointes: evaluation of a QT nomogram. QJM 2007;100(10):609–15.
32. Clemessy JL, Taboulet P, Hoffman JR, et al. Treatment of acute chloroquine poisoning: a 5-year experience. Crit Care Med 1996;24(7):1189–95.
33. Smith GD, Amos TA, Mahler R, Peters TJ. Effect of chloroquine on insulin and glucose homoeostasis in normal subjects and patients with non-insulin-dependent diabetes mellitus [Internet]. BMJ. 1987;294(6570):465–7. Available from: http://dx.doi.org/10.1136/bmj.294.6570.465
34. Powrie JK, Smith GD, Shojaee-Moradie F, Sönksen PH, Jones RH. Mode of action of chloroquine in patients with non-insulin-dependent diabetes mellitus. Am J Physiol 1991;260(6 Pt 1):E897–904.
35. Glatstein M, Scolnik D, Bentur Y. Octreotide for the treatment of sulfonylurea poisoning [Internet]. Clinical Toxicology. 2012;50(9):795–804. Available from: http://dx.doi.org/10.3109/15563650.2012.734626
36. Cole JB, Stellpflug SJ, Smith SW. Refractory Hypotension and “Ventricular Fibrillation” With Large U Waves After Overdose. JAMA Intern Med 2016;176(7):1007–9.
37. Murphy LR, Maskell KF, Kmiecik KJ, Shaffer BM. Intravenous Lipid Emulsion Use for Severe Hydroxychloroquine Toxicity. Am J Ther 2018;25(2):e273–5.
38. Bagate F, Radu C, Mekontso Dessap A, de Prost N. Early extracorporeal membrane oxygenation for cardiovascular failure in a patient with massive chloroquine poisoning. Am J Emerg Med 2017;35(2):380.e3–380.e4.
Changelog:
A previous version of the article erroneously listed the threshold QRS duration as “0.12ms” for bad outcome; this was updated to “0.12s.”