“I only have eyes for you”
Tox pupils
Author: Justin Corcoran
Internal Reviewer: Annie Arens
Why do we love the pupils in the poisoned patient? The pupil is the window to your poisoned soul. What happens to the pupils after poisoning is a wildly complicated topic masquerading as a simple outcome; they either dilate (mydriasis) or they constrict (miosis). In order to understand how toxins affect the pupils, you have to understand how the pupils work in the first place.
Overview:
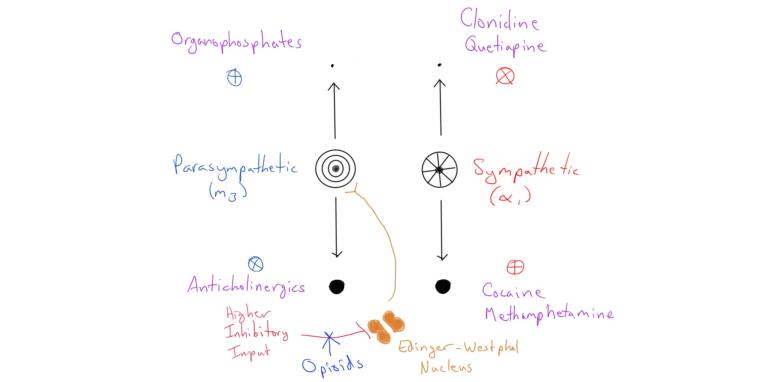
Here’s a summary overview of where we’re going:
Normal Physiology
(Hall and Chilcott, 2018)
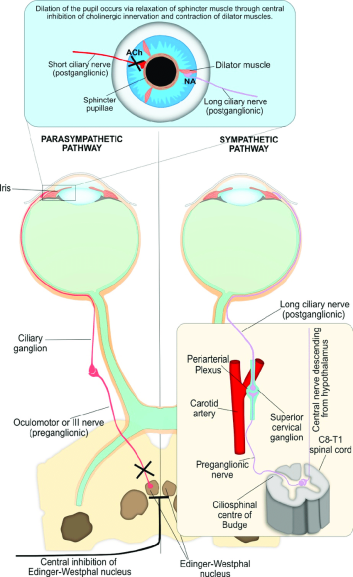
I think it’s helpful to think backwards from the site of action – in this case, the pupil. Two primary systems, the sympathetic and parasympathetic nervous system, innervate the pupil. The sympathetic innervation acts via adrenergic receptors (α1) to dilate the pupil, and the parasympathetic innervation acts via muscarinic receptor (M3) to constrict the pupil.
Upstream of the pupil, it’s important to remember that the Edinger-Westphal (EW) Nucleus, when tonically active, acts to constrict the pupil via the parasympathetic system. The EW nucleus receives higher inputs, which can be modulated as well (this is the mechanism of opioid induced miosis, which we’ll talk about later).
Toxin Induced Mydriasis

(“Mydriasis,” 2019)
It should make sense from the above discussion that there are two primary ways to produce mydriasis (agonize the alpha receptor or antagonize the muscarinic receptor).
On the adrenergic end of things, anything that produces increased circulating catecholamine should produce mydriasis. This includes things like: cocaine, amphetamine, methamphetamine, etc. Because mydriasis with these drugs is the result of excessive dilator action (the sphincter is still active), sympathomimetic induced mydriasis is classically described as reactive.
Alternatively, you have any of the antimuscarinic agents (think diphenhydramine, atropine, etc) that will produce mydriasis by blocking the acetylcholine action on the pupillary sphincter. Because mydriasis in this case is produced by knocking out the pupil’s ability to constrict (rather than increasing the dilator tone as in sympathomimetic drugs), the mydriasis associated with antimuscarinics is classically described as nonreactive.
Toxin Induced Miosis
Similar to mydriasis, there are two main ways to produce miosis, although we typically think of three: excess muscarinic tone, decreased adrenergic tone, or opioid effect.
Muscarinic excess is seen commonly in anticholinesterase drugs, such as with organophosphate or carbamate insecticides. Opioid induced miosis, while typically thought of in its own class, is actually mediated by increased muscarinic tone:
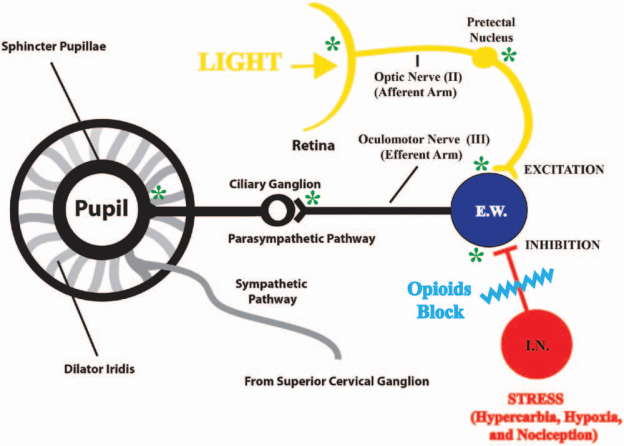
(Rollins et al., 2014)
By inhibiting the inhibitory input onto the EW nucleus, opioids allow the breaks come off – the EW nucleus is able to do what it does best, and that is constrict the iris by increasing the parasympathetic tone.
Given that adrenergic input onto the iris is mediated through an alpha-1 receptor, it should make sense that some drugs that block alpha-1 receptors (like quetiapine, olanzapine, and TCAs) can cause miosis (even when they also have anticholinergic properties as well).
Special Cases
Neuromuscular blockade
Neuromuscular blockers, in the majority of cases, DO NOT alter the pupillary response to light. A study done by Caro et al. looked at the pupillary response to light in patients who underwent RSI with either rocuronium, a non-depolarizing neuromuscular blocker, and succinylcholine (a depolarizing neuromuscular blocker). Unsurprisingly, all of the patients receiving rocuronium and most (91%) receiving succinylcholine had retained pupillary light reflex following RSI. (Caro et al., 2011)
Nystagmus
Nystagmus is an abnormal motion of the eyes which can occur in multiple directions. It is characterized by a slow drift phase followed by a rapid beat in the opposite direction; the nystagmus by convention is named after the fast-beating direction. This can occur horizontally, vertically, or in rotatory fashion. While several beats of horizontal nystagmus on lateral gaze are a normal physiologic finding, this quickly fatigues. Non-fatigable horizontal nystagmus, vertical nystagmus, and rotary nystagmus are pathologic findings.
Several common drugs produce pathologic nystagmus, the most common of which are NMDA antagonists (ketamine, dextromethorphan, and PCP) and ethanol. Ethanol frequently produces vertical and non-fatigable horizontal nystagmus, and PCP classically produces a rotary nystagmus.
Ocular Clonus
This is an abnormal eye motion which occurs in association with serotonergic toxicity. The motion is sometimes described as looking like “ping-pong balls” as it is typically multi-directional and without the slow/fast phases of nystagmus.
Fin
References:
- Caro, D.A., Andescavage, S., Akhlaghi, M., Kalynych, C., Wears, R.L., 2011. Pupillary Response to Light Is Preserved in the Majority of Patients Undergoing Rapid Sequence Intubation. Annals of Emergency Medicine 57, 234–237. https://doi.org/10.1016/j.annemergmed.2010.10.017
- Hall, C., Chilcott, R., 2018. Eyeing up the Future of the Pupillary Light Reflex in Neurodiagnostics. Diagnostics (Basel, Switzerland) 8. https://doi.org/10.3390/diagnostics8010019
- Mydriasis, 2019. Wikipedia.
- Rollins, M.D., Feiner, J.R., Lee, J.M., Shah, S., Larson, M.D.M., 2014. Pupillary effects of high-dose opioid quantified with infrared pupillometry. Anesthesiology 121, 1037–1044. https://doi.org/10.1097/aln.0000000000000384